Guest Post by By Arun Nadarasa, MRPharmS
The NHS is embarking on a transformative journey to align with its 10-Year Health Plan, an ambitious roadmap aimed at reshaping healthcare from analogue to digital, reactive to preventative, and hospital-centred to community-focused care. Central to this vision is the integration of emerging technologies like quantum computing and artificial intelligence (AI) into primary care. However, to unlock the full potential of these innovations, it’s crucial to cultivate ecosystems of collaboration, upskill the workforce in Clinical Quantum Literacy, and address regulatory and safety considerations such as Quantum as a Medical Device (QaMD) and Quantum Clinical Safety.
This article explores the role of quantum computing in healthcare transformation, the importance of creating “Menlo Park”-style innovation hubs in GP practices, and how Clinical AI and Quantum Hackathons can foster innovation. It also highlights the critical need to establish robust frameworks for safety and regulation, such as the role of Clinical Safety Officers (CSOs) in quantum-enabled care.
The NHS 10-Year Health Plan: A Vision for Change
The 10-Year Health Plan represents a bold effort to tackle longstanding healthcare challenges by embracing cutting-edge technology. It aims to digitise healthcare processes, shift focus from treatment to prevention, and decentralise care delivery. GP practices, as the backbone of community health, play a pivotal role in realising this vision. However, these practices face significant challenges, including resource constraints, workforce shortages, and inefficiencies in care delivery.
By transforming GP practices into innovation hubs—akin to the spirit of “Menlo Park,” where Thomas Edison pioneered transformative inventions—the NHS can reimagine primary care as a space for experimentation, collaboration, and the integration of advanced technologies like quantum computing and AI.
Quantum Computing in Primary Care: Unlocking New Possibilities
Quantum computing is emerging as a game-changer for healthcare, offering the computational power needed to address complex challenges that traditional systems struggle to handle. In primary care, quantum technologies can drive transformation in several key areas:
1. Quantum as a Medical Device (QaMD):
Quantum computing applications in healthcare are increasingly being recognised as potential medical devices. For example: Quantum-powered diagnostic tools that enhance imaging or identify subtle patterns in patient data.
Quantum algorithms that optimise treatment planning by simulating multiple clinical pathways.
As these tools are deployed, regulatory frameworks must ensure their safety, efficacy, and ethical use, positioning QaMD as a cornerstone of quantum integration into clinical care.
2. Enhanced Patient Pathway Analysis:
Quantum algorithms enable detailed analysis of patient journeys, improving care delivery by optimising:
Treatment timelines and resource allocation.
Geographic access to care, reducing travel-related emissions.
3. Carbon Mapping and Sustainability:
Quantum-powered models can assess and optimise the environmental footprint of healthcare operations. By reducing waste and improving energy efficiency, GP practices can contribute to the NHS’s sustainability goals.
4. Policy and Operational Modelling:
Quantum computing supports advanced healthcare policy modelling, enabling more effective resource distribution, preventative care strategies, and efficiency improvements.
The Role of Clinical Safety Officers (CSOs) in Quantum-Enabled Care
As quantum technologies are integrated into healthcare, Quantum Clinical Safety becomes paramount. Clinical Safety Officers (CSOs) will play a critical role in ensuring the safe deployment of quantum applications in clinical settings.
Quantum Clinical Safety Responsibilities:
Risk Assessment:
Evaluating the safety implications of quantum technologies, such as algorithms used in diagnostic tools or patient data analysis.
Identifying potential biases or errors in quantum systems.
Compliance with QaMD Regulations:
Ensuring quantum-powered tools meet established regulatory standards.
Collaborating with developers to address safety concerns during the design phase.
Training and Oversight:
Upskilling healthcare teams to understand and safely operate quantum-enabled tools.
Monitoring the impact of quantum applications on patient outcomes.
The integration of CSOs into quantum-enabled healthcare ensures that these powerful technologies enhance care quality without compromising patient safety.
Creating a “Menlo Park” for GP Practices
To achieve the transformative goals of the 10-Year Health Plan, GP practices must evolve into centres of innovation, research, and technological experimentation. A “Menlo Park”-style approach fosters creativity and collaboration, making primary care a hub for cutting-edge solutions.
Core Features of Innovation Hubs:
Integration of AI and Quantum Technologies:
Deploying tools like quantum diagnostics, carbon mapping, and AI-powered predictive analytics.
Collaboration Across Disciplines:
Engaging clinicians, quantum researchers, and policymakers in co-developing solutions tailored to primary care.
Workforce Development:
Prioritising Clinical Quantum Literacy to ensure healthcare professionals can leverage quantum technologies effectively.
Sustainability as a Guiding Principle:
Using quantum-powered models to enhance environmental efficiency in GP operations.
Clinical AI and Quantum Hackathons: Catalysts for Innovation
Clinical AI and Quantum Hackathons serve as powerful platforms to drive innovation in healthcare. These events bring together diverse stakeholders to tackle real-world challenges, prototype solutions, and build lasting networks of collaborators.
Key Benefits of Hackathons:
Rapid Solution Development:
Teams can develop and test prototypes addressing issues like patient flow optimisation, carbon reduction, and diagnostics.
Cross-Disciplinary Collaboration:
Clinicians, data scientists, and quantum researchers work together, combining expertise to solve complex problems.
Inspiring Quantum Integration:
Hackathons showcase the practical applications of quantum technologies, fostering confidence among NHS stakeholders in adopting these tools.
Building a Talent Pipeline:
By involving healthcare professionals in hands-on quantum projects, hackathons help develop the skills needed for future innovation.
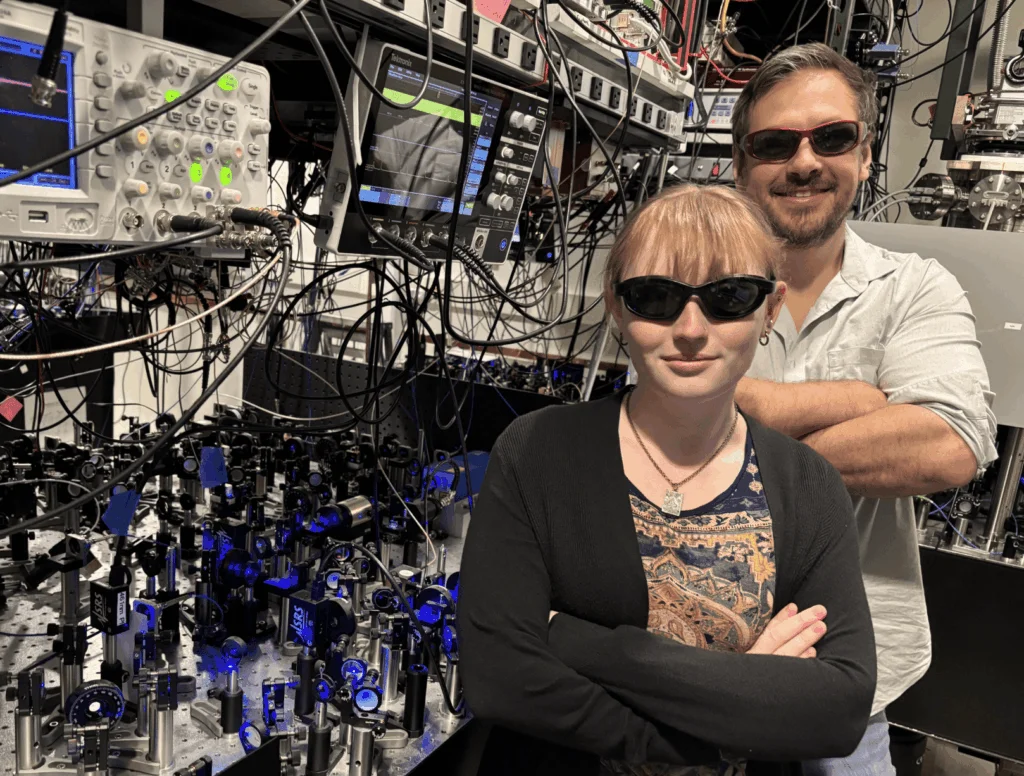
Upskilling the NHS Workforce in Clinical Quantum Literacy
The adoption of quantum computing and AI in healthcare hinges on the workforce’s ability to understand and implement these technologies. Clinical Quantum Literacy is no longer a luxury—it’s a necessity.
Key Areas of Workforce Development:
Foundational Knowledge:
Introducing healthcare professionals to quantum principles and their applications in clinical care.
Practical Skills:
Training clinicians to use quantum tools for diagnostics, resource optimisation, and sustainability efforts.
Ethics and Safety:
Equipping staff to navigate the ethical and safety challenges associated with QaMD and Quantum Clinical Safety.
Aligning with the 10-Year Health Plan
Quantum computing and AI align seamlessly with the core objectives of the NHS 10-Year Health Plan:
Analogue to Digital:
Quantum and AI technologies enable digitised diagnostics, patient journey mapping, and resource management.
Reactive to Preventative:
Predictive models support proactive care, identifying and addressing health risks before they escalate.
Hospital to Community Care:
Enhanced capabilities in GP practices reduce hospital dependency, bringing advanced care closer to patients.
Building the Future of Primary Care with Quantum and AI
The NHS is at the forefront of healthcare innovation, and quantum computing offers unprecedented opportunities to transform primary care. By establishing “Menlo Park”-style innovation hubs, fostering Clinical Quantum Literacy, and addressing safety and regulatory considerations like QaMD and Quantum Clinical Safety, we can reimagine GP practices as centres of excellence.
Events like Clinical AI and Quantum Hackathons are essential for cultivating the networks and skills needed to realise this vision. As we embrace the possibilities of quantum and AI, we must remain committed to ethical, sustainable, and patient-centred care.
The future of healthcare is not just about technology; it’s about empowering the people and systems that deliver care to adapt, innovate, and thrive. Let us seize this opportunity to shape a better, brighter future for primary care. How will you contribute to this transformation?
By Arun Nadarasa, MRPharmS
Arun is a PCN Clinical Pharmacist and an NHS Clinical Entrepreneur with a distinguished career in healthcare innovation and leadership. He is the CEO of the International Social Prescribing Pharmacy Association (ISPPA) and serves as Chair of the Pharmacy Advisory Group at the World Health Service (WHS). Arun is also the co-founder of the Clinical AI and Quantum Hackathon and the founder of the Clinical Quantum Online Course. He is the author of “Pharmacy Movement – How To Prescribe Social And Digital Medicines” and a recognised leader in social prescribing. In 2022, Arun was honoured with The Hilary International Award for Health & Care Leadership at the launch of the International Young Health Leaders Institute for his contributions to the field. This prestigious accolade also gave him the opportunity to meet and greet HRH King Charles III.